Abstract

Background:
C-CAR088, an anti-BCMA CAR T-cell therapy, is a novel 2nd generation 4-1BB chimeric antigen receptor T (CAR-T) cell therapy targeting BCMA. Previously presented results from an ongoing study of C-CAR088 in R/R MM (NCT03751293, NCT03815383, NCT04322292, NCT04295018) included a 95.7% overall response rate (ORR) for the dose of 1.0~6.0x10 6 CAR-T cells/kg with a favorable safety profile (Lu, 2020 ASH Oral Presentation #182). Here we present the updated results of the study, with more patients and longer follow up time.
Methods:
Dose escalation and expansion studies were conducted at four medical centers in China to evaluate the safety and efficacy of C-CAR088 in patients with R/R MM who were previously treated with at least 2 lines of therapy, including proteasome inhibitors (PIs) and IMiDs. C-CAR088 was administered to patients as a single infusion after lymphodepletion with fludarabine (30 mg/m 2) and cyclophosphamide (300 mg/m 2) daily for 3 days. The primary endpoint was the incidence of adverse events (AEs), including dose-limiting toxicities (DLTs), and the secondary endpoints included overall response rate(ORR), duration of response (DOR), and progression-free survival (PFS) by IMWG Uniform Response Criteria.
Results:
As of July 2nd, 2021, 31 patients had been infused with C-CAR088. The median vein-to-vein time was 18 days. The manufacturing success rate was 100%. 4, 13 and 14 patients were infused with 1.0, 3.0 and 4.5~6.0 x10 6 CAR+ T cells/kg respectively. The median follow-up time for all patients was 8.0 months (0.1-24.2). The median age of patients was 61 years (45-74). The median number of prior lines of therapy was 4 (2-13). There were 25 (80.6%) patients with at least one high risk cytogenetic abnormality and 17 (54.8%) patients with at least two high risk cytogenetic abnormalities. 7 patients (22.6%) received bridging therapy before C-CAR088 therapy.
Cytokine release syndrome (CRS) developed in 29/31 (93.5%) patients, grade 1 in 18/31 (58.1%), grade 2 in 8/31 (25.8%) and grade 3 in 3/31 (9.7%) respectively. The median time to the first onset of CRS was 6 days (1-11) and the median duration of CRS was 5 days (2-14). 9/31 (29%) patients used tocilizumab and 6/31 (19.4%) patients used corticosteroids to manage CRS. Only one patient developed a grade 1 neurotoxicity. No DLTs were observed and all adverse events were reversible. One patient died of septic shock on day 2 after receiving C-CAR088.
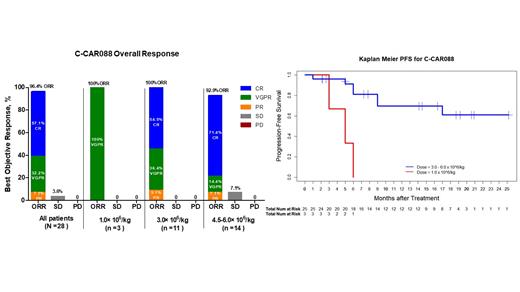
Clinical efficacy was assessed in 28 patients with ≥ 1 month of follow up. Among the 28 patients, 3, 11 and 14 patients were infused with the dose of 1.0 x 10 6 CAR+ T cells/kg 3 x10 6 CAR+ T cells/kg, and 4.5~6x10 6 CAR+ T cells/kg respectively.
The ORR was 27/28 (96.4%): 4 (14.3%) achieved CR, 12 (42.9%) achieved sCR and 9 (32.1%) achieved very good partial response (VGPR).
At the dose level of 1.0 x10 6 CAR+ T cells/kg, 3(100%) patients achieved VGPR. The median DOR was 3.7 months (1.8-5.8), and the median PFS was 4.6 months (2.7-6.2).
The CR rate was 54.5% (6/11) and 71.4% (10/14) in the 3.0 and 4.5~6.0 x10 6 CAR+ T cells/kg cohorts respectively. The median time to CR was 2.0 (0.5-9.5) months. Minimal residual disease (MRD) was testedbyEuroFlow-based flow cytometric analysis in 16 patients who had CR, 15/16 (93.7%) patients were MRD negative with the sensitivity of 10 -5. With a median follow-up of 9.5 months (1.9-24.2) in ≥ 3.0x10 6 CAR+ T cells/kg cohorts, the median DOR and PFS had not been reached. The Kaplan-Meier estimation of PFS at 6 and 12 months was 81.1% (95% CI:65.9% ~99.8%) and 69.5 % (95% CI:51.6 % ~93.6%) respectively.
8 patients in the ≥ 3.0x10 6 CAR+ T cells/kg cohorts discontinued the study. 7 discontinued due to disease progression (PD), and 1 discontinued for other anticancer therapy. 4 progressed within 6 months, 2 progressed within 6-12 months, and 1 progressed within 12-24 months.
C-CAR088 proliferated and expanded well in patients' blood. The median C max was 734,868 copies/μg gDNA. The median AUC 0~28day was 7,468,779 day·copies/μg gDNA. The median T max was 14 days. The median T last was 84 days. 71% (95% CI: 42%~92%) of patients with C max equal to or greater than the median C max achieved CR/sCR.
Conclusion:
C-CAR088 has a manageable safety profile, which includes low neurotoxicity rates (with no gr ≥3 events). Deep and durable responses were observed in ≥ 3.0x10 6 CAR-T cells/kg cohorts. Doses of 3.0 and 6.0×10 6 CAR T cells/kg were selected for further study.
Zhu: CBMG: Current Employment. Huang: CBMG: Current Employment. Li: CBMG: Current Employment. Lan: CBMG: Current Employment. Chen: CBMG: Current Employment. Humphries: CBMG Ltd: Current Employment. Yao: CBMG: Current Employment, Current holder of stock options in a privately-held company.
Author notes
 This icon denotes a clinically relevant abstract
This icon denotes a clinically relevant abstract

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal